Cereset research
HIRREM® is the Core Brain Technology Shared with Cereset®
Cereset Research is the evolution of HIRREM®, or High-resolution, Relational, Resonance-based Electroencephalic Mirroring®, which is a research technology used for specific indications, including insomnia, PTSD, concussions, hot flashes, pain, etc. The same relaxation aspects of the technology are found in HIRREM and Cereset. We are the sole developer of this advanced core technology.
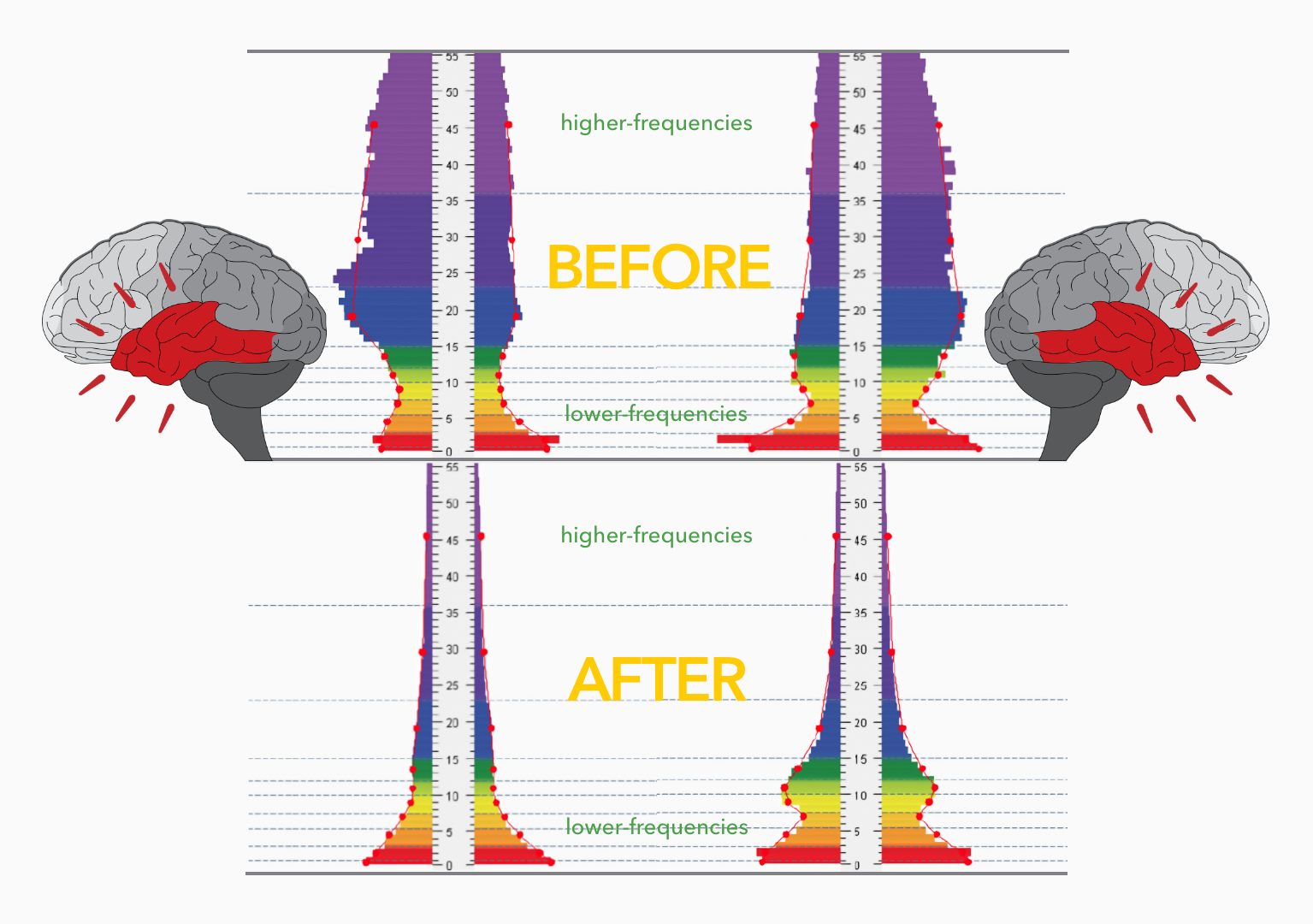
HIRREM is a precision-guided technology that permits the brain to perceive its own functionality in real time, supporting brain oscillation patterns to optimize in client-unique ways. Use of HIRREM is typically accompanied by improved sleep and other benefits. Physiological sleep is critical for health, performance, and global brain plasticity.
80+
Abstracts & Presentations
16
Peer-Reviewed Publications
9
IRB Approved Clinical Trials
1000+
Participants in Clinical Trials
HIRREM is the first and only example of closed-loop, allostatic neurotechnology. As a healthcare intervention, closed-loop, allostatic neurotechnology is a form of precision medicine for the brain. Closed-loop strategy entails monitoring brain states in real time and returning signals to the user that do not depend on clinical evaluation or conscious learning. (In contrast, open-loop approaches do not pay attention to the brain’s changing functionality; learner-in-the-loop approaches train the individual to move brain activity toward a population average.) Allostasis means “stability through change,” and it is a twenty-first century model of physiological regulation that identifies the brain as the organ of central command. (In contrast, the homeostasis idea of “stability through constancy” is based on a laboratory animal experimentation paradigm which dates to the nineteenth century.) Allostasis concords with evolutionary perspectives in biomedicine, and predicts that more optimal brain function should entail more optimal health and context-dependent performance.
Noninvasive neurotechnology from Cereset Research is being studied at the following institutions:
- Wake Forest School of Medicine, Department of Neurology, Winston-Salem, North Carolina
- Womack Army Medical Center, Fort Bragg, North Carolina.
- Uniformed Services University, Bethesda, Maryland.
Funding for this research has been provided by independent third parties including but not limited to:
- The Susanne Marcus Collins Foundation, Inc., for clinical trials to evaluate HIRREM for migraine, insomnia, and other conditions ($3 million to Wake Forest School of Medicine; 2011 – present).
- Office of the Under Secretary of Defense (Acquisition, Technology, and Logistics), to evaluate HIRREM for military personnel with traumatic stress symptoms ($107,000 to Wake Forest School of Medicine; 2014).
- United States Army Research Office, to develop Technology to Regulate Circadian Rhythm for Health and Performance, Phase I STTR Award to Brain State Technologies ($150,000; 2014).
- US Army Medical Department, Advanced Medical Technology Initiative Rapid Innovation Award to Fort Bragg, Womack Army Medical Center, to evaluate feasibility of wearable brain optimization technology in special operations personnel ($30,000 Womack Army Medical Center; 2017).
- Congressionally Directed Medical Research Programs, Psychological Health and Traumatic Brain Injury Research Program, for clinical trials to evaluate closed-loop allostatic neurotechnology for military service members with persisting symptoms after traumatic brain injury (Contract #W81XWH-17-2-0057, $2,833,185 to Brain State Technologies, with sub-awards to Geneva Foundation on behalf of Womack Army Medical Center, and Henry Jackson Foundation on behalf of Uniformed Services University).
Peer-reviewed papers have been published in the following journals:
Press Releases
SCOTTSDALE, ARIZONA (PR-WEB): 27-JAN-2023
A Natural Non-invasive Neuro-technology Improves Sleep and Wellbeing in Randomized, Controlled Clinical Trial
The Post-COVID world has an increased population suffering from sleep issues, and good sleep is the basis to good health. An insomnia intervention which is natural and non-invasive can be an important aspect to achieve improved health in a post-COVID world.
Cereset® (Ce – Cerebrum (brain) and Reset) is being used across the USA and in other countries as well as a means to provide clients a means to help reset their own brain regulation by passive listening to their own brain waves, which are translated to tones by the Cereset computer technology.
“Sleep is foundational for optimal health, healing and well-being,” said principal investigator Charles H. Tegeler, M.D., chair of neurology at Atrium Health Wake Forest Baptist, who led the team to investigate Cereset Research in a randomized controlled clinical trial. The effort compared patients with mild to moderate insomnia who listened to their own brain waves for 10 sessions of approximately an hour to those patients who were provided an active intervention using randomized tones for the same time.
The study concluded that there was a clinically significant insomnia improvement demonstrated over time by the Cereset Research group. The improvements in autonomic cardiovascular regulation were also significant for the Cereset Research group. Sleep quality, anxiety, and depression also improved. No adverse events were reported. The full study can be found in the SAGE Journal – Global Advances in Integrative Medicine and Health (https://doi.org/10.1177/27536130221147475)
“This study is a demonstration of our intent to help people help themselves and achieve a natural means to health and wellbeing,” said Lee Gerdes, Founder/CEO of Cereset. “Though we have 50 Cereset offices now in the USA, we hope to have double and triple that number in the near future to serve the many people we know have health and wellbeing compromises which we can assist them to rectify.”
Financial support for this clinical trial was supported by a research grant from The Susanne Marcus Collins Foundation, Inc. Sean L. Simpson was supported by NIBIB R01EB024559 and Wake Forest Clinical and Translational Science Institute (WF CTSI) NCATS UL1TR001420. REDCap infrastructure for data collection and management was supported by UL1TR001420.
SCOTTSDALE, ARIZONA (PRWeb): 27-JAN-2021
Cereset Research Exposes the Secrets of Traumatic Stress Hidden in the Brain
Effects of an Allostatic Closed-Loop Neurotechnology (HIRREM) on Brain Functional Connectivity Laterality in Military-Related Traumatic Stress
HIRREM® (the legacy research technology of Cereset® – a Brain State Company) was utilized by the Wake Forest School of Medicine to study symptoms of traumatic stress in military personnel before and after use of Cereset (legacy) intervention. (https://onlinelibrary.wiley.com/doi/10.1111/jon.12825)
Whole brain, resting state magnetic resonance imaging (MRI) was done pre- and post- Cereset intervention. Significant effects on brain network connectivity have been previously reported (https://onlinelibrary.wiley.com/doi/full/10.1111/jon.12571). For the current study, lateralization of brain connectivity was analyzed. Lateralization here refers to the distribution of brain connections within the right, and left side, or to the opposite side. This is important because common lobes in the right and left hemispheres of the brain execute different functions. Of note for these results, the parasympathetic division of the autonomic nervous system (which we think of as the “brake to rest and digest”) is managed primarily on the left, and the sympathetic division (which we think of as the “gas to go”) is driven primarily on the right.” Thus, the dominant left is a “freeze or numbing” response indicator, and in contrast, a dominant right is the “fight or flight” response indicator.
Funding for this study was provided by: The Susanne Marcus Collins Foundation Inc., Joint Capability Technology Demonstration Program within the Office of the Under Secretary of Defense, US Special Operations Command, and the Wake Forest Clinical and Translational Science Institute.
WINSTON-SALEM, N.C. (Wake Forrest® – Baptist Medical Center): 17-MAY-2020
Reduction in Insomnia Symptoms Associated with Non-invasive Neurotechnology
For people with chronic insomnia, a good night’s sleep is elusive. But what if insomnia symptoms could be alleviated by simply listening to one’s own brainwaves?
Researchers at Wake Forest Baptist Health conducted a clinical trial that showed reduced insomnia symptoms and improved autonomic nervous system function using a closed-loop, acoustic stimulation neurotechnology. The study is published in the September 17 online edition of the journal Brain and Behavior. “Sleep is foundational for optimal health, healing and well-being,” said principal investigator Charles H. Tegeler, M.D., chair of neurology at Wake Forest School of Medicine, part of Wake Forest Baptist Health. The study included 107 adult men and women with moderate to severe insomnia. In this study, the HIRREM participants were five times more likely than placebo to have improvement in their HRV measured as rMSSD by more than 50%. They were also twice as likely to have improved BRS by more than 50% compared to placebo.
This study was supported by a research grant from The Susanne Marcus Collins Foundation, Inc.
SCOTTSDALE, ARIZONA (PRWeb): 20-MAY-2020
Wake Forest Clinical Pilot Study Shows CERESET® Technology Supports Stress Reduction for Law Enforcement
A new clinical pilot study conducted by Wake Forest School of Medicine shows that use of a new non-invasive technology from the creators of Cereset reduces symptoms related to high stress and insomnia.
Law Enforcement has always been a highly stressful career – serving to protect, facilitate justice, and remove danger for all of us. The positions of these men and women put them constantly in harm’s way both from the criminal element as well as from the defense for not following rules precisely. Officers have always had to face very high daily stress. Now, COVID-19 introduces another even greater degree of stress as the officer may be exposing themself in the line of duty to Coronavirus and subsequently infect their loved ones. The dangers of the Coronavirus cause those who protect us to be under stress for themselves and now, also for the safety of their families and friends.
The study was led by Dr. Charles H. Tegeler, Professor and Interim Chair, Department of Neurology, and McKinney-Avant Chair in Neurology, Wake Forest School of Medicine, Winston-Salem, NC. Cereset is a Brain State Company located in Scottsdale, Arizona.
SCOTTSDALE, ARIZONA (PRWeb): 01-OCT-2019
Cereset® Announces Mild-Traumatic Brain Injury Focused Clinical Trial Progress
Results to date demonstrate that Cereset’s technology may help U.S. military personnel suffering from concussions
Cereset, the only proven non-invasive technology that helps your brain relax and reset itself, announced the midway point of its randomized research trial for individuals with persisting symptoms following mild-Traumatic Brain Injury (mTBI). The objective of the study is to measure the efficacy of a non-invasive technology which compares tones delivered to a subject’s brain guided by the brain’s own rhythms, versus random unguided tones. The research trial is being conducted in two locations–Uniformed Services University of the Health Sciences (USUHS) in Bethesda, MD; and Womack Army Medical Center (WAMC) in Fort Bragg, NC.
The impressive interim results to date, which are a combination of test and placebo, indicate a possible breakthrough for an intervention treating mTBI. Once completed, the data can be summarized in separate test and placebo results. The final report for results at the trial’s completion will provide definitive measures for the apparent positive changes seen to date.
SCOTTSDALE, ARIZONA (AAAS-EurekAlert): 21-NOV-2018
Clinical study shows Cereset® technology reduces symptoms of PTSD in military personnel
Functional Brain Network Changes Following Use of an Allostatic, Closed‐Loop, Acoustic Stimulation Neurotechnology for Military‐Related Traumatic Stress
A new clinical study conducted by Wake Forest School of Medicine shows that use of a new non-invasive technology from the creators of Cereset not only reduces symptoms of military-related traumatic stress but also improves brain function.
https://www.eurekalert.org/pub_releases/2018-11/bstl-css112118.php
WINSTON-SALEM, N.C. (Wake Forrest®- Baptist Medical Center): 15-MAY-2018
Noninvasive Brainwave Mirroring Technology Improves Heart Rate Variability
Improvements in Heart Rate Variability, Baroreflex Sensitivity, and Sleep After Use of Closed-Loop Allostatic Neurotechnology by a Heterogeneous Cohort
Use of a noninvasive, brainwave-mirroring technology significantly improved heart rate variability (HRV) for a large heterogeneous cohort, in a pilot study conducted at Wake Forest Baptist Medical Center. The study was published in the April 25 online edition of Frontiers in Public Health.
WINSTON-SALEM, N.C. (Wake Forrest®- Baptist Medical Center): 22-DEC-2017
Noninvasive Brainwave Technology Improved Post-Traumatic Stress Symptoms in Military Personnel
Successful use of closed-loop allostatic neurotechnology for post-traumatic stress symptoms in military personnel: self-reported and autonomic improvements
A noninvasive brainwave mirroring technology significantly reduced symptoms of post-traumatic stress in military personnel in a pilot study conducted at Wake Forest Baptist Medical Center. The study is published in the Dec. 22 online edition of the journal Military Medical Research.
SCOTTSDALE, ARIZONA (AAAS-EurekAlert): 6-JUN-2017
Successful clinical trial shows reduction of insomnia symptoms
HIRREM® neurotechnology better than placebo for insomnia, and improvement of autonomic cardiovascular regulation
A clinical trial has found that HIRREM® closed-loop neurotechnology is more effective than placebo at reducing symptoms of insomnia, and has additional benefits for heart rate and blood pressure regulation. Findings are being presented in Boston at the annual meeting of the Associated Professional Sleep Societies, June 3-7, 2017.
https://www.eurekalert.org/pub_releases/2017-06/bstl-bst060617.php
SCOTTSDALE, ARIZONA (AAAS-EurekAlert): 19-APR-2017
Post-traumatic stress symptoms reduced after use of HIRREM® closed-loop neurotechnology
Improvements also shown for cardiovascular system
For a series of individuals with post-traumatic stress symptoms, use of HIRREM®, an algorithm-guided neurotechnology, was associated with significant clinical improvements. Study findings were published April 19th online in BMC Psychiatry, by a team from Brain State Technologies (BST – Scottsdale, Arizona) and Wake Forest School of Medicine (Winston-Salem, North Carolina).
https://www.eurekalert.org/pub_releases/2017-04/bstl-pss041217.php
SCOTTSDALE, ARIZONA (PRWEB) SEPTEMBER 19, 2016
To Treat the Heart, Neurotechnology Aims to Balance the Brain
Announcing success in significant symptom reduction of persisting post-concussion symptoms (PPCS) with nearly all athletes returning to full participation in their competitive sport; including improvements in their reaction times.
https://www.prweb.com/releases/2016/09/prweb13693303.htm
ORLANDO, FLORIDA (AHA NEWSROOM – AMERICAN HEART ASSOCIATION) SEPT. 15, 2016
Sound therapy may balance brain signals to reduce blood pressure, migraines
American Heart Association Meeting Report Abstracts P310, P602
Study Highlights:
– A noninvasive neurotechnology that identifies and translates unbalanced brain electrical activity into audible tones was associated lower blood pressure and improved heart rate variability.
– The same technology reduced self-reported disability from migraines and associated sleep and mood disorders.
https://professional.heart.org/en/archive/archive–science-news—2016-hypertension-scientific-sessions
PUBLIC RELEASE (AAAS-EurekAlert) 16-AUG-2016
Wearable device for sleep optimization could decrease new PTSD cases in military
Analysis
Brain State Technologies® announces the presentation of a study that describes how use of a wearable neurotechnology device by military personnel could improve sleep and thereby lower the risk of developing post-traumatic stress disorder (PTSD). The ideas and analysis are being presented today at the Military Health System Research Symposium (MHSRS), being held August 15-18, in Kissimmee, Florida.
https://www.eurekalert.org/pub_releases/2016-08/bstl-wdf081616.php
PUBLIC RELEASE (AAAS-EurekAlert) 14-JUL-2016
Athletes with concussion maintain improvements after use of mirroring neurotechnology
High rate of return to play
Brain State Technologies® announces that a series of young athletes with long-term symptoms after concussion showed a variety of lasting improvements, after using HIRREM® neurotechnology. At three months, the athletes maintained their reduction of symptoms, and they had all returned to full physical exercise. The study findings were presented at the American Academy of Neurology Sports Concussion Conference that was held July 8-10, 2016 in Chicago.
https://www.eurekalert.org/pub_releases/2016-07/bstl-awc071316.php
SCOTTSDALE, ARIZONA (PRWEB) DECEMBER 31, 2015
Clinical study published evaluating Brain State Technologies’ non-invasive neurotechnology for adolescents with postural orthostatic tachycardia syndrome (POTS)
Brain State Technologies® is pleased to share news of the publication of outcomes for a series of adolescents with postural orthostatic tachycardia syndrome, or POTS, who used noninvasive neurotechnology developed by their company, in a clinical study.
https://www.prweb.com/releases/2015/12/prweb13142704.htm
SCOTTSDALE, ARIZONA (PRWEB) SEPTEMBER 28, 2015
Brain State Technologies® Successfully Produces Wearable Devices for Sleep and Performance Enhancement Under Contract with US Army Research Office
Independent clinical pilot studies have found that military personnel report robust improvements in their sleep quality when they have used the technology in an office setting.
https://www.prweb.com/releases/2015/09/prweb12973704.htm
SCOTTSDALE, ARIZONA (PRWEB) AUGUST 18, 2015
Brain State Technologies® Announces Publication of Peer-Review Article Describing New Brain-Centric Model of Education
Article describing Groundwork for Allostatic Neuro-Education (GAIN) published on August 17 in Frontiers in Psychology.
https://www.prweb.com/releases/2015/08/prweb12908659.htm
SCOTTSDALE, ARIZONA (PRWEB) FEBRUARY 19, 2015
Menopausal Women Report Improvement after Experiencing Advanced Brain Relaxation Technology
Brain State Technologies® announces publication of study reporting positive outcomes associated with use of HIRREM®.
https://www.prweb.com/releases/2015/02/prweb12526525.htm
SCOTTSDALE, ARIZONA (PRWEB) OCTOBER 24, 2014
Brain State Technologies® Announces Scientific Research Presented on the Brain’s Self-Optimizing Power to Relieve Symptoms with Migraines and Menopausal Hot Flashes
Professor Charles H. Tegeler, M.D. of Wake Forest School of Medicine shared data with the American Neurological Association on the topic of migraine headache.
https://www.prweb.com/releases/2014/10/prweb12274972.htm
SCOTTSDALE, ARIZONA (PRWEB) OCTOBER 09, 2014
Newly published Scientific Paper Offers Explanation of How Traumatic Stress Affects Health and Behavior
Brain State Technologies® announces the publication of new scientific paper in Frontiers in Psychology.
https://www.prweb.com/releases/2014/10/prweb12234484.htm
SCOTTSDALE, ARIZONA (PRWEB) APRIL 14, 2014
Brainwave Optimization Associated with Clinical Improvements After Traumatic Brain Injury
Brain State Technologies® announces the presentation of results from a case series of 21 individuals with persisting symptoms following traumatic brain injury.
https://www.prweb.com/releases/2014/04/prweb11758005.htm
SCOTTSDALE, ARIZONA (PRWEB) OCTOBER 15, 2013
Brain State Technologies® Announces Presentation of HIRREM Research Data on PTSD and Heart Rate Variability at American Neurological Association Annual Meeting
Researchers from Wake Forest School of Medicine will present research related to HIRREM®, also known as Brainwave Optimization®, to the American Neurological Association at their annual meeting on October 13-15, 2013.
https://www.prweb.com/releases/2013/10/prweb11221389.htm
SCOTTSDALE, ARIZONA (PRWEB) FEBRUARY 06, 2013
Scientists Describe Breakthrough Technology for Brain Self-Optimization in Newly Published Paper
Peer-reviewed journal Brain & Behavior publishes methodology paper on Brain State Technologies® patented approach to Brainwave Optimization®.
https://www.prweb.com/releases/2013/2/prweb10396987.htm
SCOTTSDALE, ARIZONA (PRWEB) MAY 31, 2012
Brain State Technologies® Showcases Brainwave Optimization® at International Sleep Conference
According to the National Sleep Foundation, over 54% of American adults have experienced a sleep problem sometime in their life, while the effects of sleep loss on work performance costs U.S. employers some $18 billion annually in lost productivity. Brain State Technologies® will showcase Brainwave Optimization® neuro-technology for improving brain balance at the Sleep 2012 event.
Peer-reviewed Scientific Publications Related to Cereset Research & HIRREM
Full-length Manuscripts
Tegeler CL, Munger Clary H, Shaltout HA, Simpson SL, Gerdes L, Tegeler CH. (2023). Cereset Research Standard Operating Procedures for Insomnia: A Randomized, Controlled Clinical Trial. Global Advances in Integrative Medicine and Health. 2023;12.
Tegeler CL, Munger Clary H, Shaltout HA, Simpson SL, Gerdes L, Tegeler CH. (2023). Cereset Research Standard Operating Procedures for Insomnia: A Randomized, Controlled Clinical Trial. Global Advances in Integrative Medicine and Health. 2023;12.
Dagenbach DE, Tegeler CH, Morgan AR, Laurienti PJ, Tegeler CL, Gerdes L, Lee SW, Simpson SL. (2021). Effects of an Allostatic Closed‐Loop Neurotechnology (HIRREM) on Brain Functional Connectivity Laterality in Military‐Related Traumatic StressJ Neuroimaging 2021;0:1-10.
Dagenbach DE, Tegeler CH, Morgan AR, Laurienti PJ, Tegeler CL, Gerdes L, Lee SW, Simpson SL. (2021). Effects of an Allostatic Closed‐Loop Neurotechnology (HIRREM) on Brain Functional Connectivity Laterality in Military‐Related Traumatic StressJ Neuroimaging 2021;0:1-10.
Tegeler CL, Shaltout HA, Lee SW, Simpson SL, Gerdes L, Tegeler CH (2020). High‐resolution, relational, resonance‐based, electroencephalic mirroring (HIRREM) improves symptoms and autonomic function for insomnia: A randomized, placebo‐controlled clinical trial. Brain Behav. Sep 17, 2020.
Tegeler CL, Shaltout HA, Lee SW, Simpson SL, Gerdes L, Tegeler CH (2020). High‐resolution, relational, resonance‐based, electroencephalic mirroring (HIRREM) improves symptoms and autonomic function for insomnia: A randomized, placebo‐controlled clinical trial. Brain Behav. Sep 17, 2020.
Tegeler CL, Shaltout HA, Lee SW, Simpson SL, Gerdes L, Tegeler CH (2020). Pilot Trial of a Noninvasive Closed-Loop Neurotechnology for Stress-Related Symptoms in Law Enforcement: Improvements in Self-Reported Symptoms and Autonomic Function. Global Advances in Integrative Medicine and Health 05/07/2020.
Tegeler CL, Shaltout HA, Lee SW, Simpson SL, Gerdes L, Tegeler CH (2020). Pilot Trial of a Noninvasive Closed-Loop Neurotechnology for Stress-Related Symptoms in Law Enforcement: Improvements in Self-Reported Symptoms and Autonomic Function. Global Advances in Integrative Medicine and Health 05/07/2020.
Lee SW, Laurienti PJ, Burdette JH, Tegeler CL, Morgan AR, Simpson SL, Gerdes L, Tegeler CH (2018). Functional Brain Network Changes Following Use of an Allostatic, Closed‐Loop, Acoustic Stimulation Neurotechnology for Military‐Related Traumatic Stress. J. Neuroimaging. 00:1-9. doi: 10.1111/jon.12571. Epub 2018 Oct 10.
Lee SW, Laurienti PJ, Burdette JH, Tegeler CL, Morgan AR, Simpson SL, Gerdes L, Tegeler CH (2018). Functional Brain Network Changes Following Use of an Allostatic, Closed‐Loop, Acoustic Stimulation Neurotechnology for Military‐Related Traumatic Stress. J. Neuroimaging. 00:1-9. doi: 10.1111/jon.12571. Epub 2018 Oct 10.
Shaltout HA, Lee SW, Tegeler CL, Hirsch JR, Simpson SL, Gerdes L, and Tegeler CH. (2018). Improvements in Heart Rate Variability, Baroreflex Sensitivity, and Sleep After Use of Closed-Loop Allostatic Neurotechnology by a Heterogeneous Cohort. Front. Public Health. 10:3389.
Shaltout HA, Lee SW, Tegeler CL, Hirsch JR, Simpson SL, Gerdes L, and Tegeler CH. (2018). Improvements in Heart Rate Variability, Baroreflex Sensitivity, and Sleep After Use of Closed-Loop Allostatic Neurotechnology by a Heterogeneous Cohort. Front. Public Health. 10:3389.
Tegeler CL, Gerdes L, Shaltout HA, Cook JF, Simpson SL, Lee SW and Tegeler CH. (2017). Successful use of closed-loop allostatic neurotechnology for post-traumatic stress symptoms in military personnel: self- reported and autonomic improvements. Military Medical Research. Published: 22 December 2017.
Tegeler CL, Gerdes L, Shaltout HA, Cook JF, Simpson SL, Lee SW and Tegeler CH. (2017). Successful use of closed-loop allostatic neurotechnology for post-traumatic stress symptoms in military personnel: self- reported and autonomic improvements. Military Medical Research. Published: 22 December 2017.
Tegeler CH, Cook JF, Tegeler CL, Hirsch JR, Shaltout HA, Simpson SL, Fidali B, Gerdes L, and Lee SW. (2017). Clinical, hemispheric, and autonomic changes associated with use of closed-loop, allostatic neurotechnology by a case series of individuals with self-reported symptoms of post-traumatic stress. BMC Psychiatry.
Tegeler CH, Cook JF, Tegeler CL, Hirsch JR, Shaltout HA, Simpson SL, Fidali B, Gerdes L, and Lee SW. (2017). Clinical, hemispheric, and autonomic changes associated with use of closed-loop, allostatic neurotechnology by a case series of individuals with self-reported symptoms of post-traumatic stress. BMC Psychiatry.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, Gerdes L, Shaltout HA, Miles CM, and Simpson SL. (2016). A preliminary study of the effectiveness of an allostatic, closed-loop, acoustic stimulation neurotechnology in the treatment of athletes with persisting post-concussion symptoms. Sports Medicine – Open. Published online 14 September.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, Gerdes L, Shaltout HA, Miles CM, and Simpson SL. (2016). A preliminary study of the effectiveness of an allostatic, closed-loop, acoustic stimulation neurotechnology in the treatment of athletes with persisting post-concussion symptoms. Sports Medicine – Open. Published online 14 September.
Fortunato JE, Tegeler CL, Gerdes L, Lee SW, Pajewski NM, Franco ME, Cook JF, Shaltout HA, Tegeler CH. (2016). Use of an allostatic neurotechnology by adolescents with postural orthostatic tachycardia syndrome is associated with improvements in heart rate variability and changes in temporal lobe electrical activity. Experimental Brain Research. 234(3): 791-8.
Fortunato JE, Tegeler CL, Gerdes L, Lee SW, Pajewski NM, Franco ME, Cook JF, Shaltout HA, Tegeler CH. (2016). Use of an allostatic neurotechnology by adolescents with postural orthostatic tachycardia syndrome is associated with improvements in heart rate variability and changes in temporal lobe electrical activity. Experimental Brain Research. 234(3): 791-8.
Gerdes L., Tegeler CH, and Lee SW. (2015). A groundwork for allostatic neuro-education. Front. Psychol. 6:1224.
Gerdes L., Tegeler CH, and Lee SW. (2015). A groundwork for allostatic neuro-education. Front. Psychol. 6:1224.
Tegeler CH, Shaltout HA, Tegeler CL, Gerdes L, and Lee SW. (2015). Rightward dominance in temporal high-frequency electrical asymmetry corresponds to higher resting heart rate and lower baroreflex sensitivity in a heterogeneous population. Brain Behav. 5(6): e00343.
Tegeler CH, Shaltout HA, Tegeler CL, Gerdes L, and Lee SW. (2015). Rightward dominance in temporal high-frequency electrical asymmetry corresponds to higher resting heart rate and lower baroreflex sensitivity in a heterogeneous population. Brain Behav. 5(6): e00343.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, and Pajewski NM. (2015). Reduction in menopause-related symptoms associated with use of a noninvasive neurotechnology for autocalibration of neural oscillations. Menopause. 22(6): 650-5.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, and Pajewski NM. (2015). Reduction in menopause-related symptoms associated with use of a noninvasive neurotechnology for autocalibration of neural oscillations. Menopause. 22(6): 650-5.
Lee SW, Gerdes L, Tegeler CL, Shaltout HA, and Tegeler CH. (2014). A bihemispheric autonomic model for traumatic stress effects on health and behavior. Front. Psychol. 5:843.
Lee SW, Gerdes L, Tegeler CL, Shaltout HA, and Tegeler CH. (2014). A bihemispheric autonomic model for traumatic stress effects on health and behavior. Front. Psychol. 5:843.
Gerdes L, Gerdes P, Lee SW, and Tegeler CH. (2013). HIRREM: a non-invasive, allostatic methodology for relaxation and auto-calibration of neural oscillations. Brain Behav. Mar; 3(2): 193-205.
Gerdes L, Gerdes P, Lee SW, and Tegeler CH. (2013). HIRREM: a non-invasive, allostatic methodology for relaxation and auto-calibration of neural oscillations. Brain Behav. Mar; 3(2): 193-205.
Tegeler CH, Kumar S, Conklin D, Lee SW, Gerdes EL, Turner DP, Tegeler CL, Fidali B, and Houle TT. (2012). Open label, randomized, crossover pilot trial of high resolution, relational, resonance-based, electroencephalic mirroring (HIRREM) to relieve insomnia. Brain Behav. Nov; 2(6): 814-24.
Tegeler CH, Kumar S, Conklin D, Lee SW, Gerdes EL, Turner DP, Tegeler CL, Fidali B, and Houle TT. (2012). Open label, randomized, crossover pilot trial of high resolution, relational, resonance-based, electroencephalic mirroring (HIRREM) to relieve insomnia. Brain Behav. Nov; 2(6): 814-24.
Peer-reviewed Commentary
Gerdes L. (2017). Restful Sleep for Optimum Performance and Reduction of Post-Traumatic Stress Disorder. HDIAC Journal. Winter; 3(4): 38-39.
Gerdes L. (2017). Restful Sleep for Optimum Performance and Reduction of Post-Traumatic Stress Disorder. HDIAC Journal. Winter; 3(4): 38-39.
Abstracts and Presentations
Shaltout HA, Tegeler CL, Tegeler CH. Use of a noninvasive, closed-loop, allostatic, neurotechnology reduced blood pressure and improved heart rate variability in a pre-hypertensive cohort. Poster presentation at the American Heart Association, Council on Hypertension, San Francisco CA, September 16, 2017.
Shaltout HA, Tegeler CL, Tegeler CH. Improved heart rate variability and symptoms of insomnia and stress, with use of a closed-loop allostatic neurotechnology in law enforcement officers. Poster presentation at the American Heart Association, Council on Hypertension, San Francisco CA, September 16, 2017.
Shaltout HA, Tegeler CL, Tegeler CH. Healing a broken heart using a closed-loop, allostatic neurotechnology: a case study in a patient suffering from Takotsubo Syndrome. Poster presentation at the American Heart Association, Council on Hypertension, San Francisco CA, September 16, 2017.
Tegeler CL, Howard LJ, Schmidt KD, Cook JF, Kumar S, Simpson SL, Lee SW, Gerdes L, Tegeler CH. Use of a Closed-Loop Acoustic Stimulation Neurotechnology Improves Symptoms of Moderate to Severe Insomnia: Results of a Placebo-Controlled Trial. Abstract 0389. Accepted for poster presentation at SLEEP 2017, Boston, MA, June 3-7, 2017.
Shaltout HA, Tegeler CL, Lee SW, Tegeler CH. In Subjects with Insomnia, Use of a Closed-Loop Acoustic Stimulation Neurotechnology Improves Heart Rate Variability and Baroreflex Sensitivity: Results of a Placebo-Controlled Clinical Trial. Abstract 0363. Accepted for poster presentation at SLEEP 2017, Boston, MA, June 3-7, 2017.
Nahman J, Dagenbach D, Lyday RG, Laurienti PM, Tegeler CH. Basal ganglia changes in functional connectivity and changes in anxiety. Poster presented at the annual meeting of the North Carolina Cognition Conference, UNC-Greensboro, Greensboro, NC, March 25, 2017.
Shaltout HA, Tegeler CL, Tegeler CH. Reduction of Blood Pressure and Improvement of Heart Rate Variability in Hypertensive Cohort Associated With Use of a Closed Loop Neurotechnology. P310. Accepted for poster presentation at the Hypertension 2016 Scientific Sessions, Orlando, FL, September 14-17, 2016.
Tegeler CL, Shaltout HA, Howard LJ, Tegeler CH. Improved Autonomic Cardiovascular Regulation and Reduced Symptoms Associated with Use of Closed-loop Noninvasive Neurotechnology by Healthcare Workers. P627. Accepted for poster presentation at the Hypertension 2016 Scientific Sessions, Orlando, FL, September 14-17, 2016.
Shaltout HA, Tegeler CL, Tegeler CH. Improvement of Autonomic Function and C-Reactive Protein in Military Personnel with Traumatic Stress After Use Of a Closed Loop Neurotechnology. P625. Accepted for poster presentation at the Hypertension 2016 Scientific Sessions, Orlando, FL, September 14-17, 2016.
Tegeler CL, Shaltout HA, Tegeler CH. Reduced Symptoms And Improved Heart Rate Variability Associated With Use Of Closed-Loop Noninvasive Neurotechnology By Migraineurs. P602. Accepted for poster presentation at the Hypertension 2016 Scientific Sessions, Orlando, FL, September 14-17, 2016.
Tegeler CH, Tegeler CL, Shaltout HA, Cook JF, Simpson SL. Improved symptoms, autonomic cardiovascular regulation, and function after use of a closed-loop neurotechnology for symptoms of military-related traumatic stress. Accepted for oral presentation at the 2016 Military Health System Research Symposium, Orlando/Kissimmee, FL, August 15-18, 2016.
Tegeler CH, Tegeler CL, Morgan AR, Burdette JH, Laurienti PJ. Military personnel with traumatic stress show changes in large-scale brain networks and global perfusion after use of a closed-loop neurotechnology. Accepted for poster presentation at the 2016 Military Health System Research Symposium, Orlando/Kissimmee, FL, August 15-18, 2016.
Tegeler CL, Howard LJ, Hirsch JR, Shaltout HA, Lee SW, Tegeler CH. Durability of symptom reduction and improved autonomic cardiovascular regulation after use of closed-loop neurotechnology by athletes with persisting post-concussion symptoms. Accepted for poster presentation at The Sports Concussion Conference, Chicago, IL, July 8-10, 2016.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, Shaltout HA, Laurienti PJ. Military personnel with traumatic stress show changes in large-scale brain networks after use of a closed-loop neurotechnology. Neurol. 86(S16): I7.009. Accepted for dual presentation at the American Academy of Neurology Meeting, Vancouver, BC, Canada, April 15-21, 2016.
Tegeler CH, Tegeler CL, Cook JF, Howard L, Lee S, Shaltout HA. Durability of symptom reductions associated with use of HIRREM by military personnel with traumatic stress. Neurol. 86(S16): I8.007. Data Blitz Presentations: Emerging Technologies for Neurological Research and Care, and Behavioral and Cognitive Neurology: Assessment Tools. Accepted for dual presentation at the American Academy of Neurology Meeting, Vancouver, BC, Canada, April 15-21, 2016.
Tegeler CL, Shaltout HA, Lee SW, Tegeler CH. Military personnel with traumatic stress demonstrate improved autonomic cardiovascular regulation after use of a closed loop neurotechnology. Neurol. 86(S16): P5.122. Accepted for presentation at the American Academy of Neurology Meeting, Vancouver, BC, Canada, April 15-21, 2016.
Tegeler CH et al. (2016). Military personnel with traumatic stress show changes in large-scale brain networks after use of a closed-loop neurotechnology. Accepted for American Academy of Neurology 68th Annual Meeting, Vancouver BC, Canada, Presentations: The Human Connectome: Implications for Clinical Neurology Poster Presentations, and Behavioral and Cognitive Neurology: Markers of Cognition, April 18-19, 2016.
Tegeler CH, Laurienti PJ, Tegeler CL, Shaltout HA, and Cook JF. (2015). Military personnel with traumatic stress show improved symptoms and HRV after a closed-loop neurotechnology. Accepted for Poster Presentation at AMSUS, the Society of Federal Health Professionals, San Antonio TX, December 1-4, 2015.
Tegeler CH, Laurienti PJ, Tegeler CL, Cook JF, Wistermayer PR, Lee SW, and Shaltout HA (2015). Military personnel with traumatic stress demonstrate changes in the default mode network after use of a closed-loop neurotechnology. Accepted for Poster Presentation at the American Neurological Association 2015 Annual Meeting, Chicago, September 27-29, 2015.
Tegeler CH. (2014). Use of a noninvasive neurotechnology for vasomotor symptoms. Invited lecture to the North American Menopause Society Translational Science Symposium, Washington DC, October 14, 2014.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, and Shaltout HA. (2014). Use of a closed-loop neurotechnology, HIRREM, is associated with symptom reduction and improved autonomic regulation in migraineurs. Data blitz and poster presentation at the American Neurological Association Annual Meeting, Baltimore, October 12-13, 2014.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, Gerdes L, Shaltout HA, and Miles CM. (2014). Use of HIRREM is associated with improved symptoms and neural oscillatory balance in athletes with post-concussion symptoms. Poster presentation at the American Academy of Neurology Sports Concussion Conference, Chicago IL, July 11-13, 2014.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, Franco ME, Nicholas JN, Ray CE, Howard LJ, and Shaltout HA. (2014). A noninvasive approach to improve insomnia in a military cohort. Poster presentation at the Annual Meeting of the Associated Professional Sleep Societies, Minneapolis MN, May 31 – June 4, 2014.
Tegeler CH, Tegeler CL, Cook J,F, Lee SW, Franco ME, Gerdes L, and Shaltout HA. (2014). Use of a non-invasive neurotechnology, HIRREM, is associated with improved sleep, mood, and baroreflex sensitivity in athletes with persisting post-concussion symptoms. Poster presentation at the American Academy of Neurology Annual Meeting, Philadelphia, April 26 – May 3, 2014.
Cook J, Tegeler CL, Lee SW, Shaltout HA, Franco M, and Tegeler CH. (2014). Use of a non-invasive neurotechnology, HIRREM, is associated with improved sleep and mood in a heterogeneous cohort. Poster presentation at the American Academy of Neurology Annual Meeting, Philadelphia, April 26 – May 3, 2014.
Tegeler CL, Fortunato J, Cook J, Lee SW, Franco M, and Tegeler CH. (2014). A noninvasive neurotechnology, HIRREM, is associated with symptom reduction and improved cardiovascular autonomic measures in adolescents with POTS. Poster presentation at the American Academy of Neurology Annual Meeting, Philadelphia, April 26 – May 3, 2014.
Miles CM, Tegeler CL, Lee SW, Franco ME, and Tegeler CH. (2014). A case (series) of improved symmetry. Poster presentation at the American Medical Society for Sports Medicine Annual Meeting, New Orleans, April 7, 2014.
Tegeler CH, Tegeler CL, Cook JF, Lee SW, Franco ME, Gerdes L, and Shaltout HA. (2014). Use of HIRREM, a noninvasive neurotechnology, is associated with symptom reduction and increased heart rate variability among individuals with traumatic brain injury. Podium presentation at the International Brain Injury Association, Tenth World Congress on Brain Injury, San Francisco, March 19-22, 2014.
Fortunato JE, Tegeler CL, Lee SW, Pajewski NM, Franco M, Cook JF, and Tegeler CH. (2013). Case series using high-resolution, relational, resonance-based electroencephalic mirroring (HIRREM) for POTS. Clin Auton Res. 23(5):269-70. Poster presentation at the American Autonomic Society Annual Meeting, Hawaii, October 23-26, 2013.
Tegeler CH, Tegeler CL, Lee SW, and Cook JF. (2013). High-resolution, relational, resonance-based electroencephalic mirroring (HIRREM) reduces symptoms and EEG asymmetry in an individual with PTSD. Annals of Neurology. 74(S17): S77. Poster presentation at the American Neurological Association Annual Meeting, New Orleans, October 12-15, 2013.
Tegeler CH, Tegeler CL, Lee SW, Shaltout HA, and Pajewski NM. (2013). Neural-oscillatory intervention for auto-calibration improves EEG asymmetry and heart rate variability (HRV). Annals of Neurology. 74(S17): S77. Poster presentation at the American Neurological Association Annual Meeting, New Orleans, October 12-15, 2013.
Tegeler CL, Cook JF, Lee SW, Pajewski N, Nicholas J, and Tegeler CH. (2013). Pilot study of menopause-related symptom reduction through a noninvasive EEG-based technology for auto-calibration of neural oscillations (HIRREM). Menopause. (20)12: 1356. Poster presentation at the North American Menopause Society Annual Meeting, Dallas, October 9-12, 2013.
Tegeler CH, Tegeler CL, Kumar SR, Turner DP, Gerdes L, Lee SW, and Houle TT. (2013). Randomized, placebo-controlled pilot trial of a novel, noninvasive electroencephalic feedback-based intervention, HIRREM, for alleviation of episodic migraine. Cephalalgia: Abstracts of the 2013 International Headache Conference. June; 33(8) Supplement: 99-100. Poster presentation at the International Headache Congress, Boston, June 27-30, 2013.
Tegeler CH, Lee SW, Tegeler CL, and Shaltout HA. (2013). Correlation between temporal lobe EEG asymmetry and heart rate variability. Neurology. Feb 12, 2013; 80 (Meeting abstracts 1): P03:031. Poster presentation at American Academy of Neurology Annual Meeting, San Diego, March 16-23, 2013.
Tegeler CH, Fidali B, Lee SW, Tegeler CL, and Gerdes L. (2012). Case series of PTSD symptom reduction through a new, non-invasive, EEG-based technology for facilitating self-regulation of neural oscillations (HIRREM). Poster presentation at 28th Annual Meeting of International Society for Traumatic Stress Studies, Los Angeles, Nov 1-3, 2012.
Tegeler CH, Kumar S, Conklin D, Turner D, Tegeler CL, McCall V, and Houle T. (2012). A New Method of Dynamic, Relational, Electroencephalic Auditory Feedback for Primary Insomnia. Sleep. 35, Abstract Supplement: A220. Poster presentation at the Associated Professional Sleep Societies Annual Meeting, Boston, June 9-13, 2012.
Grand Rounds and Other Invited Presentations Given by Prof. Charles Tegeler, Related to HIRREM
Reducing Insomnia and Effects of Traumatic Stress: The HIRREM Research Program. WFSM Medical Alumni Association dinner event, The Dewberry, Charleston, SC, June 22, 2017.
Closed-loop Acoustic Stimulation to Reduce Insomnia and Effects of Traumatic Stress: The WFSM HIRREM Research Program. WFSM Medical Alumni Association’s Board of Directors meeting, One Biotech Place, Winston-Salem, NC, May 13, 2017.
Closed-loop Acoustic Stimulation to Reduce Insomnia and Effects of Traumatic Stress: The WFSM HIRREM Research Program. Briefing for site visit by 8 faculty from the University of Virginia School of Medicine Contemplative Sciences Center, WFSM, Winston-Salem, NC, March 24, 2017.
Closed-loop Acoustic Stimulation to Reduce Insomnia and Effects of Traumatic Stress: The WFSM HIRREM Research Program. Briefing for Sheriff Bill Schatzman, Forsyth County Sheriff’s Office, and 10 of his leadership team, Winston-Salem, NC, March 17, 2017.
Closed-loop Acoustic Stimulation to Reduce Insomnia and Effects of Traumatic Stress: The WFSM HIRREM Research Program. Briefing for Chief Barry Rountree, Winston-Salem Police Department, and 15 members of his leadership team, Winston-Salem, NC, March 9, 2017.
Closed-loop Acoustic Stimulation for Auto-calibration of Oscillating Neural Circuits: The WFSM HIRREM Research Program. Briefing/Site Visit by Semper Fi and NICOE, WFSM, February 17th, 2017.
Closed-loop Acoustic Stimulation for Auto-calibration of Oscillating Neural Circuits: The WFSM HIRREM Research Program. Neurology Grand Rounds, UT-Memphis, Memphis, TN, January 27, 2017.
HIRREM Research at WFSM: Overview of Method, Results, and Opportunities. Office of Development and Alumni Affairs, WFSM, November 11, 2016.
HIRREM Research at Wake Forest School of Medicine (WFSM): Overview and Focus on Military Traumatic Stress, Briefing for Site Visitors from Womack Army Medical Center, and USASOC, at Fort Bragg, NC, August 24, 2016.
Closed-loop Acoustic Stimulation for Auto-calibration of Oscillating Neural Circuits: Overview and Focus on Military Traumatic Stress, Neurology Grand Rounds, University of Texas Health Science Center-San Antonio, San Antonio, TX, July 29, 2016.
Durability of Symptom Reductions Associated with Use of HIRREM by Military Personnel with Traumatic Stress. Medical, Biomedical, & Biodefense: Support to the Warfighter Symposium, Raleigh, NC, June 8, 2016.
HIRREM: Overview and Focus on Military Traumatic Stress, Palliative Care Symposium, Body, Mind, & Spirit, Spartanburg Regional Healthcare System, Spartanburg, SC, May 13, 2016.
HIRREM Research at WFSM: Focus on PTSD and Military Traumatic Stress, Sci-Works After Dark, Sci- Works, Winston-Salem, NC, February 23, 2016.
HIRREM Research at WFSM: Focus on Military Traumatic Stress, Department of Family and Community Medicine, Resident Lecture Series, Winston-Salem, NC, February 10, 2016.
HIRREM Research at WFSM: Focus on Military Traumatic Stress, Department of Psychiatry Grand Rounds, Winston-Salem, NC, November 6, 2015.
Balancing the Brain by Feedback with Auditory Tones, Sci-Works Science Café, Clemmons, NC, October 27, 2015.
Overview of HIRREM and Research Program at WFSM, Neuroscience Graduate Students lecture series, Winston-Salem, NC, October 27, 2015.
HIRREM Research Overview, for Hypertension and Vascular Research Center retreat, Winston-Salem, NC, June 22, 2015.
ANS Brain Balance & Dominance: Stress, Depression, & Sleep, for an IGNITE Conference on Autonomic Nervous System and Aging, Sticht Center on Aging, Winston-Salem, NC, March 16, 2015.
Overview of HIRREM and Research Program at WFSM, for Grand Rounds, Center for Health and Healing, Spartanburg Regional Healthcare System, Spartanburg, SC, January 21, 2015.
Noninvasive Neurotechnology (HIRREM) for Vasomotor Symptoms, for The Science of Thermoregulation and Vasomotor Symptoms: New Targets for Research and Treatment, The 2nd Utian Translational Symposium, Washington, DC, October 14, 2014.
Case Series of HIRREM for Mild TBI, for North Carolina Military Business Center Conference, Raleigh, NC, June 5, 2014.
HIRREM at Wake Forest School of Medicine: Overview and Research Update, for Grand Rounds in the Hypertension and Vascular Research Center at Wake Forest School of Medicine, February 26, 2014.
HIRREM at WFSM: Overview and Potential Military Relevance, for a NC Military Foundation/Marines Special Operations Command briefing, Raleigh, NC, February 24, 2014.
Balance and Neural Oscillations. Key Note Presentation, Healing Without Borders Annual Meeting, Denver, CO, October 5, 2013.
Traumatic Brain Injury/Concussion: A Clinician’s Perspective. MS1 Neuroscience Block, WFSM, April 2, 2013.
HIRREM at WFSM: Update on Clinical Research Outcomes. Office of Women in Medicine and Science Seminar Series, Wake Forest Baptist Health (WFBH), March 6, 2013.
HIRREM at WFSM: Overview and initial Clinical Research. Wake Forest University (WFU) Sports Medicine Staff Conference, WFU, December 4, 2012.
HIRREM at WFSM: Overview and Recent Military Experience. North Carolina (NC) Military Foundation Board of Directors, Chapel Hill, NC, December 3, 2012.
HIRREM at WFSM: Overview and Initial Experience. WFBH Department of Psychiatry Grand Rounds, WFBH, November 16, 2012.
HIRREM at WFSM: Overview for US SOCOM. Special Operations Command, McDill, AFB, October 30, 2012.
HIRREM at WFBH: Overview and Initial Clinical Research. Neuroscience Postgraduate Program Tutorial, WFBH, October 5, 2012.
HIRREM at WFBH: Overview and Initial Clinical Research. Sports Medicine Section meeting, WFBH, September 19, 2012.
HIRREM at WFBH: Program Development and Initial Clinical Research. Kansas University Medical Center, TBI Research Working Group, web presentation, August 30, 2012.
HIRREM at WFBH: Overview and Initial Clinical Research. Center for Integrative Medicine, Spartanburg Regional Medical Center, Spartanburg, SC, August 23, 2012.
BioBiz Partnering Forum, Winston-Salem, NC, June 28, 2012.
HIRREM for Insomnia: Results of a Pilot Clinical Trial. Grand Rounds for Hispanics in Research Capability, University of Puerto Rico, School of Health Professions, San Juan, PR, May 21-22, 2012.
HIRREM for Migraine: Overview and Initial Results of a Pilot Clinical Trial. Action Health, Winston- Salem, NC, March 26, 2012.
HIRREM for Insomnia: Results of a Pilot Clinical Trial. Sticht Center Conference on Aging, WFBH, February 8, 2012.
CIM Update: High-resolution, Relational, Resonance-based, Electroenchephalic Mirroring (HIRREM). CIM Steering Committee Meeting, WFSM, December 12, 2011.
Brainwave Optimization for Insomnia: Results of a Pilot Clinical Trial. Neurology Grand Rounds, WFSM, November 1, 2011.
Other Selected Presentations by Brain State Technologies
Advancing Concussion Management through Innovative Technology. Sung Lee, Discussant. Annual Assembly of the American Academy of Physical Medicine and Rehabilitation, Denver, Colorado, October 14, 2017.
Sleep Quality and Risk for Subsequent PTSD: Implications for a Realistic Primary Prevention Strategy. Sung Lee. Presentation for Annual Meeting of the Society for Brain Mapping and Therapeutics, Los Angeles, California, April 19, 2017.
Moving the Needle on “Brain Enhancement”: Remediation of PTSD and TBI Symptomatology After Use of a Noninvasive Closed-Loop Neurotechnology. Sung Lee. Presentation for Annual Meeting of the Society for Brain Mapping and Therapeutics, Miami, Florida, April 9, 2016.
The Brain Creates. Lee Gerdes and Sung Lee, Presentation for W.O.N.D.E.R. Project Lecture Series, Foundation for Living Medicine, Arizona Science Center, Phoenix, Arizona, September 11, 2015.
The Brain as the Organ of Central Command: Implications for Health Strategies. Sung Lee and Charles Tegeler, Grand Rounds Presentation at Gibbs Cancer Center, Spartanburg Regional Healthcare System, Spartanburg, South Carolina, January 20, 2015.
Introduction to Brainwave Optimization. Lee Gerdes and Sung Lee, Presentation to introduce Community Mental Health Demonstration Project led by Ujima Enterprises, Kalamazoo, Michigan, July 25, 2011.
Can Brain-Balancing Technology Reduce Recidivism? Lee Gerdes and Sung Lee, Special Presentation to Idaho Criminal Justice Commission, Boise, ID, May 21, 2010.